|
Haemodialysis is a treatment
for those patients whose
kidneys cannot function any
more. It is a way of
cleansing the blood of
toxins, extra salts and
fluids through a dialysis
machine called "artificial
kidney". It helps maintain
proper chemical balance such
as potassium, sodium and
chloride and keeps blood
pressure under control.
During dialysis, two needles
will be placed into the
vascular access, one to
remove the blood and the
other to return cleansed
blood to the body. You are
connected (via tubing) to
the dialysis machine through
a vein in your arm, the
blood is pumped from your
body to a special filter
called the dialyser, which
is made of tiny capillaries.
Blood is continuously pumped
through the dialyser, where
waste products and excess
water are removed. The blood
becomes purified when the
waste products diffuse from
the blood across the
membrane of these tiny
capillaries. This purified
blood is then returned to
your body through larger
tubes.
Haemodialysis is performed 3
times a week, with each
session lasting about 3 to 5
hours, depending on the body
size and medical condition.
At the NKF, patients can
choose Mondays, Wednesdays
and Fridays or Tuesdays,
Thursdays and Saturdays.
They can also choose the
morning, afternoon or
evening session.
Before and during dialysis,
you need to clean the skin
covering the access before
inserting the needles to
avoid infection. If you
notice any signs of
infection, inform the nurse
immediately. Besides, you
need to make sure that your
blood is flowing and not
clotting while on treatment,
lightly touch the area to
feel a pulse. It is
important that the catheter
be kept dry, even when you
are taking a bath.
You also need to take care
of your fistula or graft.
You should not wear anything
tight around the
fistula/graft arm i.e.
watches, bracelets, tight
clothing, or carry heavy
bags looped over the
fistula/graft. Despite of
checking that the
fistula/graft is working by
feeling for the buzzing
sensation every morning and
night, you should not allow
non-dialysis staff to take
blood or blood pressure on
your fistula/graft arm.
Observe for signs of
infection, such as redness,
oozing of blood or pus,
swelling and heat, you need
to contact the nurse
immediately if there are any
problems with your
fistula/graft.
|
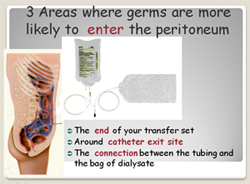
What is Peritoneal
Dialysis?
Peritoneal dialysis (PD) is
an alternative treatment to
haemo-dialysis. A special
sterile fluid is introduced
into the abdomen through a
permanent tube that is
placed in the peritoneal
cavity. The fluid circulates
through abdomen to draw
impurities from surrounding
blood vessels in the
peritoneum, and it is then
drained from the body.
PD can be carried out at
home, at work, or on trips,
but requires careful
supervision. PD gives
patients more control.
However, they need to work
closely with the health care
team including the
nephrologist, dialysis
nurse, dialysis technician,
dietitian and social worker.
The role of the PD patient
and his/her family are very
important. By learning more
about the treatment,
patients can work with the
health care team to achieve
the best possible results
and lead an active life.
The walls of the abdominal
cavity are lined with a
membrane called the
peritoneum, which allows
waste products and extra
fluid to pass from your
blood into the dialysis
solution. In PD, a soft tube
called a catheter is used to
fill the abdomen with a
cleansing liquid called
dialysis solution. The
solution contains a type of
sugar called dextrose that
will pull waste and extra
fluid into the abdominal
cavity, will be exuded out
of the body when the
dialysis solution is
drained. The used solution
will be thrown away.
The process of draining and
filling is called an
exchange and takes about 30
to 40 minutes. The period
when the dialysis solution
is in the abdomen is called
the dwell time. A typical
schedule calls for four
exchanges a day, each with a
dwell time of 4 to 6 hours.
Different types of PD have
different schedules of daily
exchanges. |
APD is suggested to offer a
number of unproven
psychosocial benefits over
CAPD. It relates directly to
fewer connections and allows
patient to lead a normal
lifestyle during the day,
particularly for workers,
school pupils and those
taking care of the elderly
or debilitated patients.
Additional benefits include
the absence of fluid during
the day, which possibly
reduces back pain and body
image difficulties.
Performing APD at night in
the supine position also
results in reduced
intra-abdominal pressures as
compared with the upright
position in CAPD. |
|
APD is designed to be simple
and is often performed in
the bedroom. The machines
are user-friendly. Before
going to sleep, the machine
needs to be loaded with
fluid. It will then perform
a number of cycles
throughout the night. The
fluid is drained away into a
large drainage bag for
disposal. Often, the machine
will provide a last fill of
fluid, which stays inside
the tummy until the
following night when it is
drained away.
Peritoneal dialysis units
worldwide are increasingly
adopting APD. It is
estimated that one quarter
of the world's peritoneal
dialysis patients are now on
APD. The use of cyclers in
North America has increased
from 10% in 1990 to 43% in
1997. 60% of patients
treated with APD in North
America also receive at
least one exchange during
the day. APD is more
expensive than CAPD, but is
usually cheaper than a
transfer to in-centre
Haemodialysis.
To see if the exchanges are
removing enough waste
products such as urea,
several tests must be
performed regularly. These
tests are especially
important during the first
weeks of dialysis to
determine whether the
patient is receiving an
adequate amount or dose of
dialysis.
The peritoneal equilibration
test measures how much sugar
has been absorbed from a bag
of infused dialysis solution
and how much urea and
creatinine have entered into
the solution during the
4-hour exchange.
In the clearance test,
samples of used solution
drained over a 24-hour
period are collected, and a
blood sample is obtained
during the day when the used
solution is collected. The
amount of urea in the used
solution is compared with
the amount in the blood to
see how effective the PD
schedule is in removing urea
from the blood.
From the used solution,
urine and blood
measurements, the health
care team can compute a urea
clearance rate called Kt/V
and a creatinine clearance
rate. The residual clearance
of the kidneys is also
considered. These
measurements will show
whether the PD prescription
is adequate. If the
laboratory results show that
the dialysis schedule is not
removing enough urea and
creatinine, the doctor can
change the prescription. |



 PERITONEAL DIALYSIS
PERITONEAL DIALYSIS
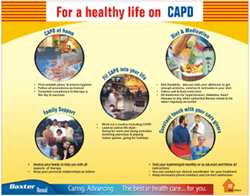 Healthy Life on CAPD
Healthy Life on CAPD